Utah Behavioral Health Accepts New Challenges
The Substance Abuse and Mental Health Services Administration (SAMHSA), an agency within the U.S. Department of Health and Human Services conducted a study which revealed that 22.4 percent of the adult population for Utah behavioral health, experienced a mental disorder in the past year.
Out of those people, 5.14 percent had a severe mental disorder. Utah had the highest percentage in the United States compared to the national average of 18.3 percent. The study overall estimated that 42.5 million people over the age of 18 in the U.S. had experienced a mental illness in the past year. Severe mental illness affected 9.3 million people, a rate of 4 percent.
The factors that contribute to the variations among states are not well understood and will need further study.
NAMI
The National Alliance on Mental Illness (NAMI) Utah’s mission is to ensure the dignity and improve the lives of those who live with mental illness and their families through support, education, and advocacy.
NAMI’s inception in 1979 established itself as a grassroots mental health advocacy dedicated to improving the lives of individuals and families affected by mental illness. Utah is considered the number one state of giving generously, and due in large to these donations from individuals, corporations, and foundations, NAMI Utah has been able to build on its success. Promoting awareness about mental illness and promoting the promise of recovery.
NAMI also offers education and support programs to engage in support networks and collaboration.
Utah Behavioral Health
Utah behavioral health leaders have the vision to take on the challenges that come with the identification and treatment of mental illnesses and addictions.
It becomes an opportunity to integrate large bodies of knowledge in a process known as “consilience,” wherein human service agencies, health care, social services, schools, and the office of justice and prisons have previously been divided into silos of truly helping the mentally ill patient to a great loss and disadvantage. When we can integrate the framework and foundation of all human systems, the results shift from “treatment to healing.”
Considering the additional social determinants to “health” within the multiple ways that class, race, and socioeconomic status interact with the mentally ill and social health, we understand the need for integration along with a true continuum of care.
We cannot go on just treating the resulting illnesses and behaviors presented by behavioral health patients, i.e., substance abuse, lack of attachment, and other medical and mental health issues, but must pay attention to the underlying core cause of all of these.
When we address the core trauma and find collaboration within all human services, private and public, then we will spend less money, help more people, and have better outcomes (McFeature, B. & Herron-McFeature, C., 2017).
Division of Substance Abuse and Mental Health
The Division of Substance Abuse and Mental Health supports the Department of Human Service Model of Care and mission to strengthen lives by providing children, youth families and adults individualized services to thrive in their homes, schools, and communities.
The five pillars of the model of care are Prevention, Operational Excellence, People and Culture, Self-Reliance, and Partnership.
It should be noted that Governor Herbert’s 2017 budget included:
- Medicaid Match for Local Mental Health Authorities. $4,400,000 one-time funding and $2,000,000 ongoing funding.
- $450,000 one-time backfill for Medicaid Expansion fund.
- Jail-Based Forensic Competency Restoration $3,300,000 in ongoing funding.
- Drug Court Treatment – Backfill Decline in Earmarked Tobacco Settlement Funds of $1,204,200.
For more information go to the 2016 Executive Summary Report at https://dsamh.utah.gov/pdf/Annual%20Reports/2016%20Executive%20Summary%20Final%20Web.pdf
Utah Division of Substance Abuse and Mental Health
The Utah Division of Substance Abuse and Mental Health (DSAMH) is also dedicated to promoting a trauma-informed approach in the public substance use disorder and mental health system.
Since 2009, they sponsored training and conferences which focused on trauma; trauma-informed care; trauma-specific interventions and gender responsive services.
According to the National Center for Mental Health Promotion and Youth Violence Prevention, over 60 percent of adults report experiencing abuse or other difficult family circumstances during childhood.
Twenty-six (26) percent of children in the United States will witness or experience a traumatic event before they turn four. When working with people with a chronic mental illness, you will find many times it is scored in underlying chronic distress from a history of trauma-exposure.
Intermountain Healthcare
Intermountain Healthcare is a Utah-based, not-for-profit system of 22 hospitals, a Medical Group with more than 1,600 physicians and advanced practice clinicians at about 180 clinics, a health plans division called SelectHealth, and other health services.
Intermountain Healthcare has integrated mental health by introducing the Mental Health Integration (MHI) approach to healthcare which focuses on both mental and physical health needs. It all takes place at the primary care clinics offering a “one stop shop.”
The Mental Health Integration Team includes:
- The patient and family member(s)
- The primary care physician
- Mental health provider (psychologist or social worker)
- Care manager or health advocate (nurse or medical assistant)
- Psychiatrist or psychiatric APRN. All team members communicate and work together.
Family Healthcare in Southwest Utah a Federally Qualified Health Centers (FQHC), also offers full integration with licensed behavioral health clinicians on site.
For more information on this visit Agency for Healthcare Research and Quality at https://www.ahrq.gov/, The goal of integrating behavioral health in primary care clinics is to treat the whole person. True integration involves care coordination across all disciplines and is very complex based on the history of the “silo” effect of services.
To provide a true continuum of care is the key to improved patient experience and health outcomes.
Federally Qualified Health Centers
Federally Qualified Health Centers offer provisions which support the enhancement of integration and coordinated effort between primary care and behavioral health providers, and to collaborate with specialty mental health systems addressing major psychiatric disorders associated with comorbid medical conditions.
The Integrated Behavioral Health Model of Care has shown to decrease depression levels in comorbid medical and behavioral health conditions, and overall health improvement outcomes. The Integrated Behavioral Health Model has also reflected cost effectiveness, i.e., a decrease in ER visits and reduced medical care utilization with patients who possess high-risk comorbid conditions (McFeature, B. & Herron-McFeature, C., 2017).
There is a growing consensus on the benefits of mental health integration which is leading to medical schools to rewrite their curricula.
Certifications and Higher Education opportunities, just to name a few, are currently being offered at: Radford University, University of Massachusetts Medical School (UMASS), and Arizona State University (ASU) who is offering a Doctor of Behavioral Health (DBH), which prepares graduates to deliver integrated behavioral care treatment programs in primary care and other medical settings.
RWJF
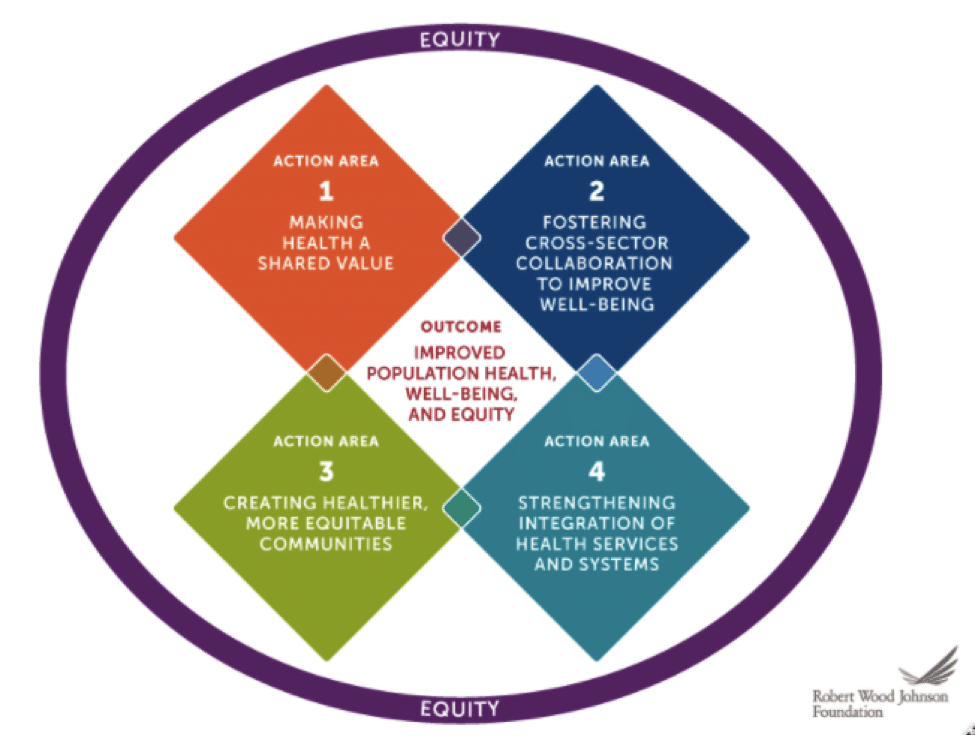
The Robert Wood Johnson Foundation (RWJF) looked at building a “Culture of Health,” wherein every person has an equal opportunity to live the healthiest life they can – regardless of where they may live, how much they earn, or the color of their skin.
With this new vision for a “healthy population,” it will require all of the sectors to come together to find ways to solve the interconnected problems.
The development of a new Culture of Health Action Framework developed in collaboration with the RAND Corporation using research data and input from individuals, leaders, and organizations across the USA.
The framework translated a broad range of sectors and developed a Culture of Health into four interconnected Action Areas listed on the chart below.
With the message of a “culture of health” and a patient centered focus the health care system will help more people and reflect a positive direction to offer clinical best practices.
With resources to support behavioral health staff working in integrated primary care clinics to enhance their role on the primary care team. An integrative behavioral health program development will meet the needs of the patient population seen for depression, anxiety and pain syndromes.
Insterested in learning more about Utah Behavioral Health? Are you looking for help? New Roads can help! Contact us today, (888) 358-8998 or email info@newroadstreatment.com
Cinthia McFeature, Ph.D.
Bill McFeature, Ph.D.
Resources and References
Agency for Healthcare Research and Quality (AHRQ) at http://intergrationacademy.ahrq.gov/
For more information on a Culture of Health visit
http://www.cultureofhealth.org/
For more information on Family Healthcare in Southwest Utah visit
http://www.familyhc.org/
For more information on Intermountain Healthcare visit
https://intermountainhealthcare.org/
McFeature, B. & Herron-McFeature, C. (2017). Integrated Healthcare HeartPath Practitioner Assessment and Intervention for the Trauma-Exposed Patient. Welbourne, FL: Motivational Press, Inc.
SAMSHA/HRSA Center for Integrated Health Solutions data retrieved from www.integration.samhsa.gov/