The stigma of mental illness is one of the major challenges we continue to face today.
The 1999 Surgeon General highlighted shame, stigma, and discrimination as major reasons why people with mental health problems avoid seeking treatment.
According to the American Psychological Association, they found that close to one-third (30%) of adult respondents were concerned about others learning about their mental health treatment, and one-fifth (20%) identified stigma as a reason for not seeking a mental health professional.
Therefore, someone who is dealing with depression may not seek mental health treatment due to the “shame” associated with mental illness. Don’t let the stigma of mental illness keep you from getting help.
A study, published Feb. 25, 2014, in Psychological Medicine, the researchers collected information from 144 studies involving 90,000 people around the world. The results of the study showed that “Stigma” ranked as the fourth highest of 10 barriers to care.
Others were afraid to let anyone know they have a mental health issue or were concerned about confidentiality.
Warning Signs of Clinical Depression
If you suspect that a friend or family member is struggling with depression, you may recommend that they go to their primary care provider. Research has shown that most people will go to their primary care provider due to the stigma of going to a “mental health provider.”
The warning signs of depression appear in the physical body, mental state, emotional response, and spiritual health.
Some of the signs are as follows:
#1. Physical Body
- Insomnia (early-morning wakefulness or sleeping too much).
- Aches and pains that don’t go away, i.e., headaches, muscle pain, cramps.
- Overeating or appetite loss.
- Digestive problems that don’t get better even with treatment.
- Severe fatigue.
#2. Mental State
- Trouble concentrating, remembering details, and making decisions.
- Short-term memory loss or confusion.
- Negative perceptions of everything and thoughts of suicide.
- Loss of interest in things that were once pleasurable, including sex.
#3. Emotional Response
- Feelings of guilt, worthlessness, and helplessness.
- Irritability with daily life stressors and relationships.
- Persistent sadness, anxiety, or “empty feelings.”
- Pessimism with regards to daily and future life plans.
#4. Spiritual Health
- Feeling hopeless and like the “Divine Source” doesn’t care.
- Religion becomes a source of guilt and shame.
The Stigma of Mental Illness & Warning Signs in Social Media
It is also important to consider that we live in an age of social media and selfies.
Therefore, if you read some of the narratives written on Facebook, Instagram, Twitter, etc. you can read between the lines and see the cry for help, for example,
“I give up on everything.” or “I am always alone.”
If you read narratives/posts which mention some of the warning signs of depression or other serious mental illness you may be the one person who checks on the individual by phone or in person.
When the social media postings are blatantly threatening or post disturbing pictures, i.e., dead frogs, guns or ammunition this should be reported to someone who can get help. Reportedly depression played a factor in the recent school shooting in Florida for Nickolas Cruz.
However, the presentation of depression symptomatology, in this case, is only the “peak of the iceberg.”
This seventeen-year-old adolescent had many loss factors in his life, including his father, Roger Cruz – who along with his wife, Lynda had adopted Nikolas and then died of a heart attack several years ago. Then in November 2017, his mother, Lynda Cruz, 68, died of pneumonia. With her death, Cruz and his half-brother lost one of the only relatives they had left. The “perfect storm” came together with a combination of feelings of rejection, depression, grief from the loss of family, and possible history of exposure to trauma (unknown). Cruz marched through Marjory Stoneman Douglas High School, killing 17 people and wounding at least 15 others.
According to the Washington Post, February 15th, 2018, Mackenzie Hill, a 17-year-old junior at Stoneman Douglas, stated that she had known Cruz since middle school and that he was always getting into trouble. Hill, like others, also cited Instagram posts, which in the wake of the killings, Israel called “very, very disturbing.”
An Instagram account that allegedly appeared to belong to the suspect showed several photos of guns. And one appeared to show a gun’s holographic laser sight pointed at a neighborhood street. A second showed at least six rifles and handguns laid out on a bed with the caption “arsenal.” Other pictures showed a box of large-caliber rounds with the caption “cost me $30.” One appeared to show a dead frog’s bloodied body. Most of the photos were reportedly posted in July.
How to Prepare a Friend or Family Member to Get Professional Help
To prepare a friend or family member to go to their primary care provider, you can tell them that it might be a good idea to get a physical and share some of the symptoms they have been experiencing with a medical professional.
You can tell explain to them that the primary care provider will want to know:
- When the symptoms began
- How long have they lasted
- How severe are they, i.e., on a scale of 1-10 with 1 being not too bad and 10 being extremely hard and may have experienced a trip to the emergency room.
- Does depression or other mental illnesses run in your family
- Do you have a history of drug or alcohol abuse?
Integrated Primary Care Team Approach for Assessing and Treating Depression
Some of the primary care outpatient clinics offer same-day service for the patient who enters a primary care clinic. Same-day service means that the clinic has a primary team approach providing behavioral health consultants to work with the primary care providers.
This integrative system allows key components to take place as follows:
- Population health based framework that allows co-location of behavioral health consultants within the clinic walls
- Identifying the patient’s needs which in turn allow the primary care team (PCP-BHC coordinated care) to develop critical pathways that speak to each patient’s medical condition. A holistic health approach (mind, body, and spirit) is utilized aligning with primary care philosophy.
The integrated primary care philosophy in a “team care approach” includes daily team meetings sometimes referred to as “huddles,” embedded behaviorists, training interns, and behaviorists that are accessible to the primary care team.
With the primary care team approach, the patient experience of care is improved, the patient understands prevention and interventions necessary for improving overall health, and there is no “stigma” attached to mental health because it is about the patient’s health.
The primary care team become the frontline treatment providers in primary care settings to screen and provide health-related plans to address both acute (prevention) and chronic medical conditions that associate with either or both mental and emotional difficulties.
The patient makes an appointment with the medical provider (PCP). The potential patient enters the lobby area of the clinic and greeted by the front desk staff.
The patient is called back to the nursing station or exam room where vitals are measured and recorded by the MA/LPN nursing staff who conducts the standard health status examination (weight measure, blood pressure, pulse/heart rate) and acquires the medical information with the administration of particular questionnaires.
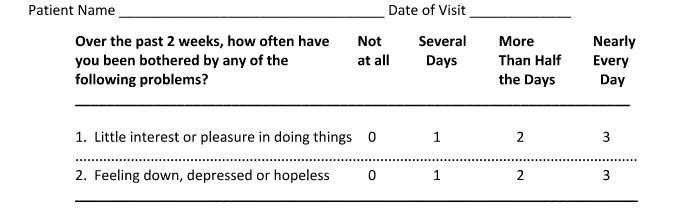
These include the PHQ-2 (brief screening measure for depression) seen chart below.
The PHQ-2 self-report above inquiries about the frequency of depressed mood and anhedonia over the past two weeks. The PHQ-2 includes the first two items of the PHQ-9.
The purpose of the PHQ-2 is not to establish a final diagnosis or to monitor depression severity, but rather to screen for depression in a “first step” approach. Patients who screen positive should be further evaluated with the PHQ-9 to determine whether they meet criteria for a depressive disorder. When scoring the PHQ-2, the range is from 0-6.
The authors identified a PHQ-2 cutoff score of 3 as the optimal cut point for screening purposes and stated that a cut point of 2 would enhance sensitivity, whereas a cut point of 4 would improve specificity.
The PHQ-9, AUDIT-C, and Cage-A may also be utilized to further screen if needed. The PHQ-2 and PHQ-9 are depression measures, and the AUDIT-C and Cage-A are alcohol and drug measures.
Suicide Prevention & the Stigma of Mental Health
We know that depression is a leading factor in suicide and affects about 90% of people who kill themselves.
However, depression is certainly not the only reason people harm themselves. A person with a history of traumatic life events, social rejection, chronic illness, and a host of other factors can contribute to a person considering or attempting suicide.
If you suspect that someone is suicidal, it is important to take the following precautions and get the individual help. Do not leave someone you suspect is suicidal alone. If the person attempts to harm themselves, call 9-1-1 or emergency services in your area. You should also alert a family member or friend as soon as possible. If you’re not with the person, tell them to call the National Suicide Hotline at 800-273-TALK (800-273-8255).
If you’re outside the United States, look for the equivalent in your country. A suicidal person needs professional intervention as soon as possible.
What Can We Do to Help?
We can all help by paying attention to the warning signs of depression or someone in need of help. When you take the time to actively listen to someone from “your heart” and “their heart” you may hear a story that is woven in despairing words.
Don’t be afraid of the stigma of mental health. it’s okay.
Listening is a simple act of kindness.
When we listen to people, they will know they are not alone, and there is always help and someone who understands the pain of depression and other mental illness. We need to be careful not to allow our hearts to become hardened and be mindful of the devastation of depression and other mental illnesses when left untreated.
Be Present and Mindful
In this busy world of technology and globalization, we must take time to ground ourselves. We must be present and mindful so that when someone is crying out for help, we hear them. Think of the loss of so many innocent lives that did not need to happen if someone truly listened and saw the warning signs of mental illness.
“It’s only with the heart that one can see rightly; what is essential is invisible to the eye.”
-Antoine De Saint-Exupery
At New Roads Behavioral Health we focus on mental health & BDT through a program that we offer called, WORTH.
DBT was developed specifically to provide that kind of support and is widely recognized as one of the most useful treatments for borderline individuals.All of our WoRTH therapists have been extensively trained, at the Portland DBT Institute. We emphasize DBT for all our clients–even those without BPD–due to the broad scope of its treatment potential.
To get more information about WORTH and other treatment please fill out a form and contact us here.