Are you fighting an opioid addiction?
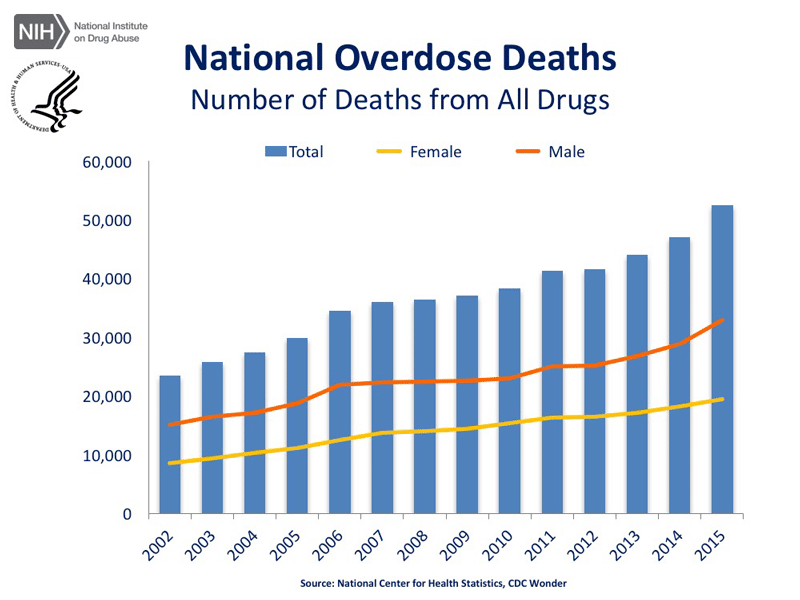
Drug overdose is the leading cause of accidental death in the US, with 52,404 lethal drug overdoses in 2015. Opioid addiction is driving this epidemic, with 20,101 overdose deaths related to prescription pain relievers, and 12,990 overdose deaths related to heroin in 2015.
Human beings are always searching for ways to alleviate pain. Individuals from all walks of life have become dependent on prescription pain medication containing opioids.
The focus is now on the opioid addiction epidemic and what needs to be done to stop the increasing deaths from prescription pain medication.
According to the Department of Health and Human Services (HHS) the United States is in the midst of an “unprecedented” opioid epidemic. Since 1999, the rate of overdose deaths involving opioids including prescription opioid pain relievers and heroin have nearly quadrupled with over 165,000 people who have died from prescription opioid overdoses.
In March 2015, HHS Secretary Sylvia M. Burwell announced an initiative targeting three priority areas to tackle the opioid epidemic;
- Prevention
- Treatment
- Research
#1. Prevention
Prevention such as; improving prescribing practices, considering “outside the box” supplements and other complimentary medicine.
#2. Treatment
Treatment such as; integrating mental health services in primary care, medication- assisted treatment, utilization of cognitive behavioral therapy (CBT).
In CBT, substance use is viewed as an intrapersonal and interpersonal issue, a relapsing and habitual disorder that can be successfully treated. Also, inpatient and outpatient substance abuse interventions, and consideration of treating the “whole” person.
#3. Research
Research to study alternatives to prescription pain medication with opioids and expanding the use of naloxone to prevent overdoses.
“Investigating, understanding,
and embracing our deepest pain
are the first steps on the path
to transforming our pain to power.”
-Daniel Beaty
Much of prevention involves educating patients about pain and the different qualities and causes of pain.
Pain is considered a submodality of somatic sensation and it is often used to describe a wide range of physical and emotional pain experiences. These experiences may be associated with actual or potential tissue damage.
Pain becomes information transmitted to the central nervous system to elicit fight or flight. It also warns of us that our mind and body needs attention and may require additional evaluation by medical and behavioral health care providers. Most illness will cause various types of pain and the ability to diagnose different diseases depends to a great extent on the knowledge of the different qualities and causes of pain.
Sensitivity and reactivity to noxious stimuli are essential to the well-being and survival of an organism.
Pain travels through redundant pathways, ensuring to inform the subject: “Get out of this situation immediately.”
Without these attributes, the organism has no means to prevent or minimize tissue injury. Individuals congenitally insensitive to pain are easily injured and most of them die at an early age (Yang, P.B., et.al. 2006).
Assessment and Treatment
A pain questionnaire is another tool that helps to illustrate for patient pain levels and track and monitor.
Most of the time in the busy primary care setting it is easiest to use the scaling question about pain levels on a scale of 0 – 10. There are, however, more detailed pain questionnaires.
In primary care settings when a patient has been prescribed opioid prescription pain medication or may be prescribed pain medication a more detailed pain questionnaire such as the Opioid Risk Tool may be administered.
The Opioid Risk Tool (ORT) is a brief, self-report screening tool designed for use with adult patients in primary care settings to assess risk for opioid abuse among individuals prescribed opioids for treatment of chronic pain.
The ORT can be administered and scored in less than a 1 minute and has been validated in both male and female patients, but not in non-pain populations.
This questionnaire was developed by Lynn R. Webster, M.D. to assess the risk of opioid addiction. Considered high risk factors for opioid abuse are: family history of substance abuse (alcohol, illegal drugs and RX drugs), personal history of substance abuse, history of preadolescent sexual abuse, and psychological disease (ADD, OCD, bipolar, schizophrenia, depression).
Develop a Plan of Care for Chronic Pain Syndromes (Example)
- Discuss with the patient what they feel contributes to the pain.
- Questions like: “Where is the pain located?” and, “What is the frequency, duration, and causes of the onset of the pain?” You might also use the scaling questions for pain levels, “On a scale of 1 to 10, 1 being mild pain and 10 being excruciating pain, what is your pain level now?”
- Address areas of emotional pain and anxiety with the patient. Ask if the patient if they would be willing to provide a brief narrative about life events that they remember. When conducting a narrative assessment, it will bring to life the patterns and themes which may be contributing to the pain.
- Discuss self-management strategies and reflect all of the healthy actions that the patient is doing to have less pain.
- Pain management requires discipline, patience, and determination. Reflect the importance of attitude towards the pain that will assist with the patient’s perception of the pain.
- Spiritual practices and guided imagery can assist with reduction of the pain. You may want to introduce guided imagery that utilizes self-biofeedback and helps the patient learn to listen to their body.
Some of the activities which may be helpful for the patient would be walking/light exercise, massage, acupuncture, stretching, ice/heat, breathing exercises, yoga, meditation, and craniosacral therapy.
Also, other activities that may help the patient keep their mind off the pain include crafts, coloring, reading and helping others in some capacity.
The patient must be the one to consider what is realistic, affordable, and doable for them, and must be something they enjoy.
Research
Research has shown that when people transition from an acute injury or illness to chronic pain, it is due to central sensitization (Arendt-Nielsen, et al., 2003).
Central sensitization is associated with chronic pain in which the nervous system becomes stuck and in a state of heightened reactivity.
In central sensitization, the sensations of pain can be more intense even to the sensation of touch or massage. Central sensitization maintains the pain after an initial injury or illness heals.
Recent discoveries about how the body detects, transmits and reacts to painful stimuli, have allowed physicians to relieve both acute and chronic pain.
Massive advances have been made in our understanding of the pharmacology of the opioid systems but despite this and the considerable effort expended in developing new and more selective molecules, there has been a disappointing lack of significant progress towards the Holy Grail of opioid research, that is, the development of a powerful analgesic drug, free from the undesirable effects of morphine.
It may be that new drugs for the relief of pain will act through mechanisms unrelated to the opioid system, as exemplified by gabapentin, originally developed as an anticonvulsant (Corbett, A.D., et al., 2006).
Research on mindfulness continues and is offering patients alternatives to treating pain with medication only.
Medication typically only helps reduce pain about 20% so managing the pain involves a menu of interventions to treat the “whole person.” Daniel Siegel has researched mindfulness and the application to a nonlinear, moment-to-moment integrative and transformative psychotherapy.
Once a patient experiences the essence of mindfulness with gratitude it is life enhancing and allows self-actualization and transcendence to occur, unencumbered by pain.
Take a breath and open the door to your heart and know that life is a gift, so get the help that you need today with your opioid addiction.
The New Roads team wants to help you, alongside with Eric Schmidt who is an expert in opioid addiction.
Call us today! (888) 358-8998
Cinthia McFeature, Ph.D.
Learn about the opioid addiction epidemic here, from Eric Schmidt himself.
References
Arendt-Nielsen, L. & Graven-Nielsen, T. (2003). Central sensitization in fibromyalgia and other
musculoskeletal disorders. Current Pain & Headache Reports, 7, 355-361.
Corbett A. D., Henderson G., McKnight A.T., Paterson S.J. 75 years of opioid research: the exciting but vain quest for the Holy Grail. British Journal of Pharmacology. 2006;147(Suppl1):S153-S162.
McFeature, B. & Herron-McFeature, C. (2017). Integrated health – HeartPath practitioner assessment and intervention for the trauma-exposed patient. Melbourne, FL: Motivational Press, Inc.
Siegel, D. J. (1999). The developing mind. How relationships and the brain interact to shape who we are. New York: Guilford Press.
Yang, P.B., Swann, A.C. and Dafny, N. Sensory evoked potentials recording from the ventral tegmental area, nucleus accumbens, prefrontal cortex and caudate and locomotor activity are modulated in dose response characteristics by methylphenidate. Brain Res. 1073:164-174, 2006.